You are here

Surgery, chemotherapy, radiotherapy and, during the past few decades, targeted and immunotherapies… the therapeutic arsenal deployed to fight cancer has never been so extensive. The problem is that like bacteria, which may become impervious to antibiotics, cancer cells can also develop “resistance” to cancer treatments and elude them. Overcoming this phenomenon is therefore crucial to improving the long-term survival of patients.
A molecule that has been developed in Lyon, (southeastern France), could help to address this challenge. And it would be “universal” to all types of current chemical cancer treatments. “The result of two decades of research, our molecule has proved very promising during two studies, which we published in August 2023”12, rejoyces Patrick Mehlen, director of the Cancer Research Centre of Lyon (CRCL)3. “This potential new treatment offers a new and original therapeutic approach. We haven’t yet won the battle. But we are very hopeful that we will see it enrich the therapeutic arsenal and improve the fight against various cancers that are currently very difficult to treat,” comments Éric Solary, a scientist at the Institut Gustave Roussy’s AMMICA laboratory4, and member of the Board of the ARC foundation for cancer research.
A therapeutic antibody
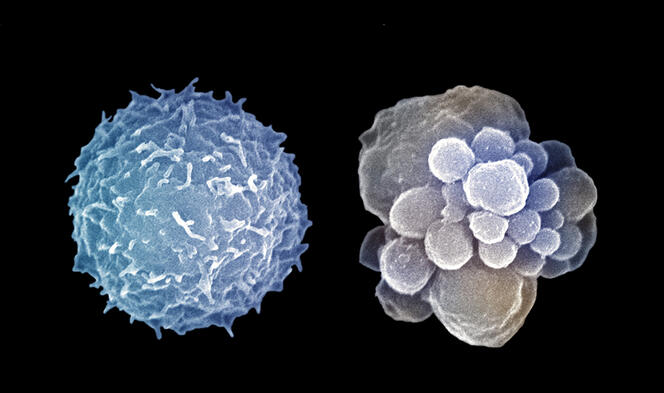
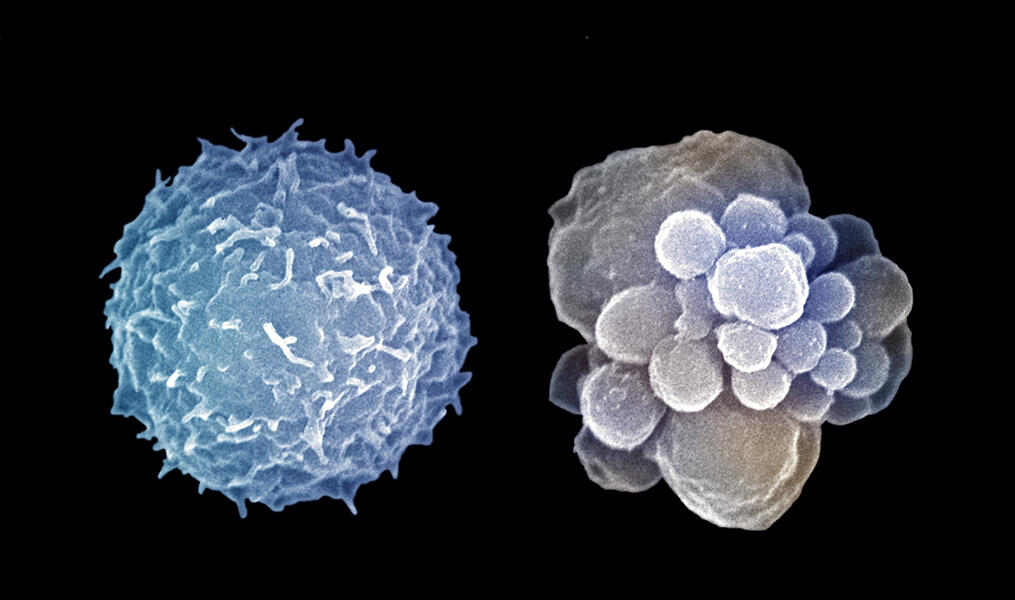
What does this mean in practice? A monoclonal antibody (produced in the laboratory) called NP137. “Like the antibodies produced by our immune system during an infection, this one is able to block a specific compound. In this case, it is not a viral or bacterial molecule, but a protein called netrin-1 that is present in most cancers,” Mehlen explains. The fascinating scientific process that led to this compound started more than twenty years ago, when the Lyon biologist and his team were working on a mechanism that is defective in cancer cells: programmed cell death (or apoptosis), which allows infected or abnormal cells to self-destruct. The researchers were particularly interested in a cell receptor that can induce apoptosis, a protein called DCC5, identified initially during studies on colon tumours. This receptor can indeed be blocked by the famous netrin-1 protein, which is the preferred target of the NP137 antibody… hence the team’s interest in this molecule.
During initial trials in the mouse that were published in 20046, the team made a significant discovery: while netrin-1 is mainly known to guide the development of neurons in an embryo, they found that in adults it could also favour the onset of colorectal cancer. Over the years, the Lyon scientists were able to provide proof of the involvement of netrin-1 in several other types of so-called “solid” cancers (breast, lung, skin, etc.) and “liquid” cancers (affecting elements of the blood, such as lymphoma). It thus occurred to them that they could block netrin-1 in order to kill cancer cells. Their concept became reality in 2014 with the development of the NP137 antibody, thanks to funds raised by Netris-Pharma, a medical start-up created in 2008. Finally, following preclinical studies in the mouse and having obtained the necessary authorisations, in 2017 the group initiated the first study designed to test this antibody in humans. It is the findings of this phase I trial involving 14 female patients with advanced cancer of the endometrium (the inner wall of the uterus) that were described in one of the two surveys published last August7.
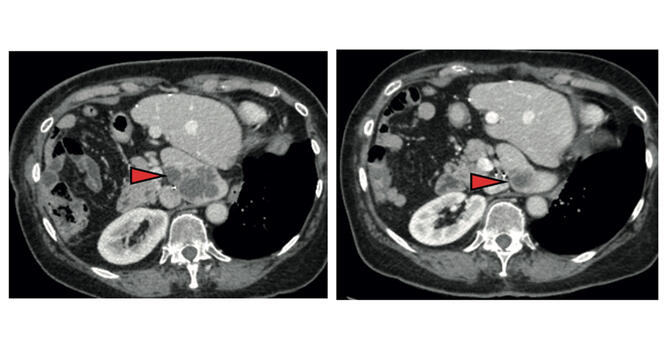
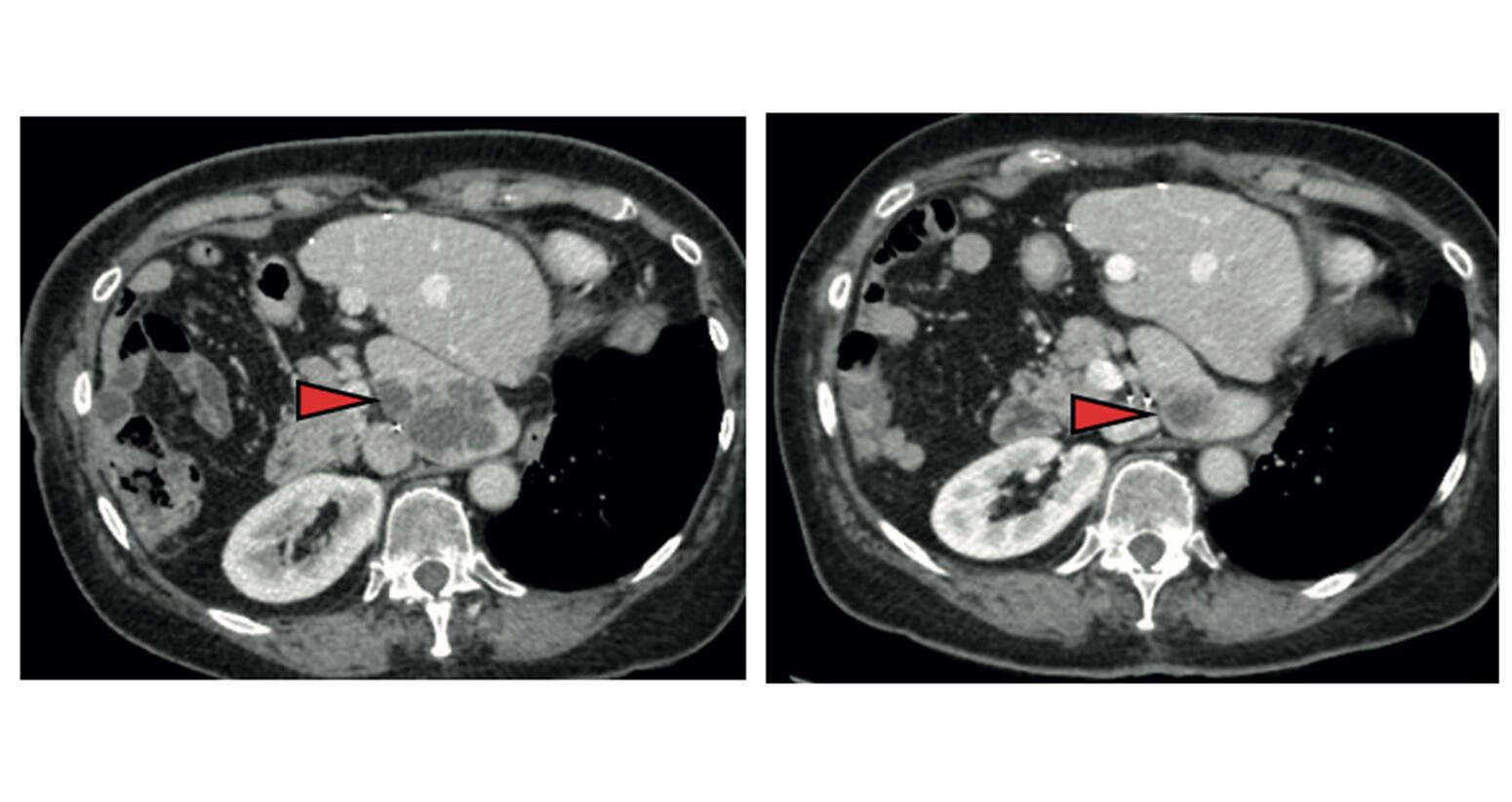
The outcome showed not only that NP137 was non-toxic but it was also able to halt progression of the disease in more than half of the patients (8 out of 14). Better still, after six weeks of treatment, the scientists saw in one of them a reduction of more than 50% in metastases, the tumours that develop in other organs from the primary tumour in the endometrium. Based on these results, the scientists turned to mice with endometrial cancer and administered NP137 combined with chemotherapy (carboplatin-paclitaxel). This combination proved to be more effective than chemotherapy alone. Not only did it enable a reduction in tumours but it could potentially offset their resistance to treatment.
Promising results
And this was not limited to chemotherapy! According to more recent studies in the mouse8 published in October 2023, NP137 may also attenuate resistance to immunotherapy treatments. In an effort to elucidate the underlying process, a second study published in August 20239 was led jointly by Mehlen and Cédric Blanpain, a scientist at the ULB in Brussels (Belgium). The team performed several cell biology and genetics experiments in mice affected by epidermoid skin cancer (a severe form of cancer) and on human tumour cells. This work ultimately showed that the blockade of netrin-1 by the NP137 antibody was able to thwart one of the principal mechanisms of tumour resistance: the epithelial-mesenchymal transition.
This transition allows proliferating cancer cells to change their status and acquire the ability to “break down” the substrate on which they are lying, the extracellular matrix. These cells subsequently have access to the rest of the body via the circulatory system and can thus metastasise and become impervious to treatments. “The latter – called mesenchymal cells – tend to multiply less, which renders them less susceptible to chemotherapy. In addition, they produce molecules that hide them, and inhibit the immune system, thus making them resistant to immunotherapy,” explains Mehlen. “Targeting this epithelial-mesenchymal transition has been an important goal that numerous scientists have been focusing on for many years, and Mehlen’s team is the first to have achieved it, thanks to NP137,” adds Solary.



It is nevertheless necessary to verify via rigorous trials that this antibody can indeed inhibit the resistance phenomenon in humans. “That’s precisely the main challenge of four new clinical studies – phase 2 this time – which are under way and target several types of cancer,” reveals Mehlen. Called “GyNET”, one study involves nearly 240 women with endometrial or advanced cervical cancer who are being treated in 15 French centres. They are receiving standard chemotherapy alone or chemotherapy and/or immunotherapy, both combined with NP137. The other three clinical trials should include a total of around 200 patients. One general study focusing on patients resistant to immunotherapy, whatever their cancer; the second on pancreatic cancer and the third on liver cancer. The aim is to verify that this antibody enhances the efficacy of the treatments to which it is added.
The results of these different studies should become available in the coming months. “If they are conclusive, we can move on to phase 3 trials to confirm the benefit of this antibody in more patients (up to 500) and to apply for a marketing authorisation,” states Mehlen. If all goes well, he says, the health authorities may approve the wider use of NP137 by 2026. This could significantly enhance the therapeutic arsenal to fight cancer.♦
See on our website:
Cancer: the immunotherapy revolution
- 1. P. A. Cassier et al., Nature, 2 August 2023, doi: 10.1038/s41586-023-06367-z
- 2. J. Legrand et al., Nature, 2 August 2023, doi: 10.1038/s41586-023-06372-2
- 3. CNRS / INSERM /Université Claude Bernard Lyon 1 / Centre Léon Bérard.
- 4. Analyse Moléculaire, Modélisation et Imagerie de la Maladie Cancéreuse (CNRS / INSERM / Institut Gustave Roussy / Université Paris-Saclay).
- 5. “Deleted in Colorectal Cancer”.
- 6. L. Mazelin et al. Nature. 2 September 2004. doi: 10.1038/nature02788.
- 7. P. A. Cassier et al., op cit, 2023.
- 8. B. Ducarouge et al. Cell Death Differ. October 2023. doi: 10.1038/s41418-023-01209-x.
- 9. J. Legrand et al., 2023, op. cit.
Keywords
Share this article
Author
A freelance science journalist for ten years, Kheira Bettayeb specializes in the fields of medicine, biology, neuroscience, zoology, astronomy, physics and technology. She writes primarily for prominent national (France) magazines.















Comments
Log in, join the CNRS News community